CASE STUDY
Health system boosts MA revenue 5% by closing compliance gaps.
Ensemble improves Two-Midnight Rule adherence and accountability from Medicare Advantage payers.
SNAPSHOT
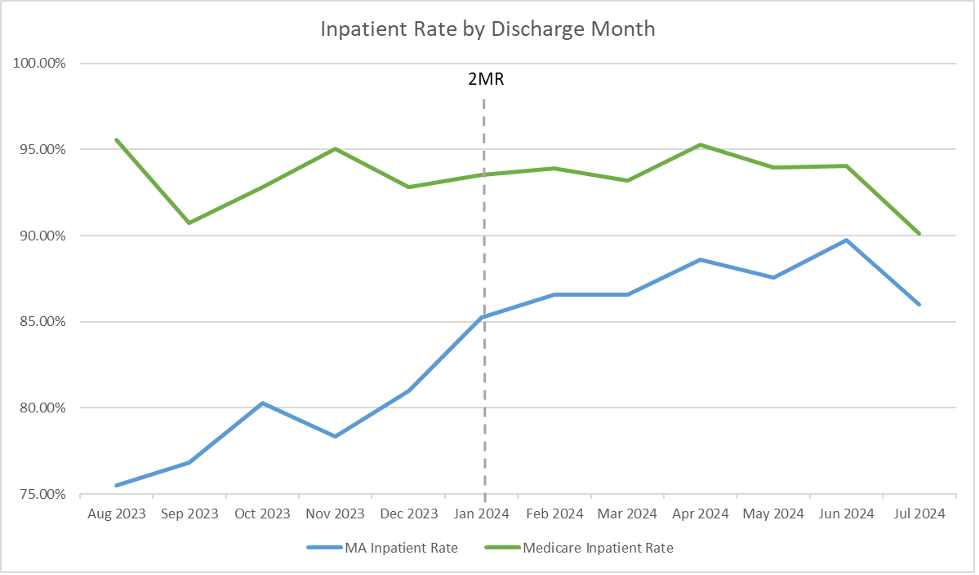
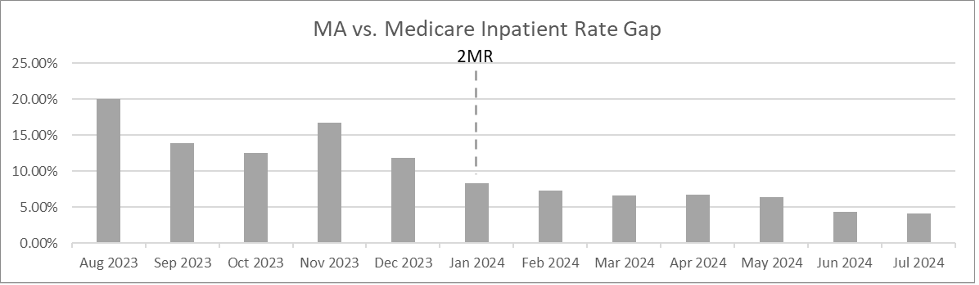
To support Medicare Advantage (MA) payer compliance with the CMS Two-Midnight Rule and address differences in performance between traditional Medicare and MA, a large health system collaborated with Ensemble to enhance utilization management processes, including the introduction of peer-to-peer reviews. Over a period of seven months, this approach resulted in an 11.5% increase in inpatient MA admission ratios, stable initial denial rates and a 5% rise in revenue per account.
PROFILE
- Health system
- > $4B NPR
- 20+ hospitals
- Midwest
- End-to-end RCM partner since March 2016
Challenges
This system faced mounting operational and financial strain due to inconsistent Medicare Advantage admission criteria and vague documentation standards. Payer variability and misalignment with CMS’s Two-Midnight Rule led to inefficiencies, reimbursement uncertainty, and increased administrative overhead,” creating performance gaps versus traditional Medicare that demanded resolution to protect margins and stabilize revenue.
Solutions
To address the inconsistencies in Medicare Advantage admissions and improve alignment with payers, Ensemble introduced a framework to support clinical decision-making, clarify and optimize documentation requirements and workflows and align operational practices with regulatory standards. As part of this framework, a targeted metric was introduced to the payer scorecard to measure and report differences in admission rates between Medicare and Medicare Advantage, reinforcing accountability and visibility. This comprehensive approach helped reduce performance gaps compared to traditional Medicare.
What we did:
-
Educated providers on CMS criteria
Delivered targeted education to clinical teams to ensure accurate documentation and alignment with CMS’s Two-Midnight Rule requirements. -
Ensured documentation quality and claim readiness
Focused on front-end documentation and claim preparation to avoid spikes in denials, enabling smoother reimbursement for newly admitted cases. -
Optimized admission decision protocols
Refined UM workflows to identify qualifying cases for inpatient admission under the Two-Midnight Rule, reducing variability across payers. -
Implemented Physician Advisory program
Implemented a thorough and scalable physician advisory program leveraging Ensemble’s clinical experts to support peer-to-peer reviews with payers to help explain clinical decision-making and defend inpatient status when appropriate.
When your UM foundation is solid — strong documentation, educated providers and a disciplined peer-to-peer process — you can be more assertive with admissions. You’re not gambling on outcomes; you’re executing with confidence.
Brad Gingerich, Vice President, Revenue Cycle Operations, Payer Strategy
Results
Maintained first-pass denial rates despite aggressive approach to admissions
Protected cash velocity for inpatient Medicare Advantage cases
